Reflections on this past year 2019 (and decade)
“Joy comes from having a relationship with the unchanging God and transcends any trial we can face on this earth” – Jeremy Camp
Dear friends,
I’m a few days late on this annual “reflections” blogpost because I haven’t been feeling my “normal” (more on that at the end of this post).
Anyways, 2019 is now over, and along with that, another decade has passed. I have so many mixed emotions about this.
I’ve realized that it’s now been a whole decade since all of my health issues started. This recap is going to be a little long (or should I say really
long ), so feel free to skim or skip altogether and just scroll down to the end for the current update. I just want to document all of this as it is kind of like my medical journal and also a place for me to share all my thoughts.
), so feel free to skim or skip altogether and just scroll down to the end for the current update. I just want to document all of this as it is kind of like my medical journal and also a place for me to share all my thoughts.
2010: At age 17, I had surgery on the bottom of my right foot to remove a vascular malformation that I was born with. Throughout the years leading up to it, there were numerous times when I couldn’t walk on it because it caused so much pain. Little did we know that once I had the surgery, things were never the same.
2011: Even after my foot healed from the surgery, the pain never went away and got more severe by the month (my foot was cold to the touch, the coloring of it was green and purple, and even the slightest touch caused horrible pain). My pediatrician referred me to OHSU’s Comprehensive Pain Center where I met my pain dr. (to this day, he is my favorite doctor ever ). He diagnosed me with Complex Regional Pain Syndrome (also known as Reflex Sympathetic Dystrophy). I started aggressive physical therapy to “desensitize” the pain and had to stick my foot in all kinds of things like uncooked rice, small gadgets, buttons, uncooked pasta, etc. to help my body/nervous system get used to that kind of physical contact. I even had to start mirror therapy (what amputees use when they have phantom pain) to “trick” my brain into thinking it’s the same as my left foot. All of that intensive therapy never helped (and the CRPS eventually spread to my left foot), so I had another surgery to get a “spinal cord stimulator” implanted in my back. There were “leads” connected to the actual implant that were placed near my spinal cord. They sent different “impulses/sensations” down my legs and into both feet that “blocked” the pain signals. It was so amazing, and I could finally walk after being on crutches for more than a year. While the SCS helped the pain in my feet, the CRPS spread to my left hand that November after a simple prick to my finger to draw a little blood for routine blood work that my pediatrician ordered.
). He diagnosed me with Complex Regional Pain Syndrome (also known as Reflex Sympathetic Dystrophy). I started aggressive physical therapy to “desensitize” the pain and had to stick my foot in all kinds of things like uncooked rice, small gadgets, buttons, uncooked pasta, etc. to help my body/nervous system get used to that kind of physical contact. I even had to start mirror therapy (what amputees use when they have phantom pain) to “trick” my brain into thinking it’s the same as my left foot. All of that intensive therapy never helped (and the CRPS eventually spread to my left foot), so I had another surgery to get a “spinal cord stimulator” implanted in my back. There were “leads” connected to the actual implant that were placed near my spinal cord. They sent different “impulses/sensations” down my legs and into both feet that “blocked” the pain signals. It was so amazing, and I could finally walk after being on crutches for more than a year. While the SCS helped the pain in my feet, the CRPS spread to my left hand that November after a simple prick to my finger to draw a little blood for routine blood work that my pediatrician ordered. Because the SCS only helped from the legs down, I had to start aggressive hand therapy to keep the CRPS from progressing. CRPS spreading to more than one limb is not common, and my pain dr. was convinced something underlying was going on..
Because the SCS only helped from the legs down, I had to start aggressive hand therapy to keep the CRPS from progressing. CRPS spreading to more than one limb is not common, and my pain dr. was convinced something underlying was going on..
2012: At the beginning of 2012, I started experiencing more symptoms like low blood pressure, light headedness, joint subluxations, etc. So after more doctor visits, I was diagnosed with Postural Orthostatic Tachycardia Syndrome and Ehlers-Danlos Syndrome Type 3. But those diagnoses weren’t too “disabling” which I was very thankful for. In July of that year, my family went to Eagle Crest for summer vacation. One of those days, my siblings and I challenged ourselves and went on a long, mainly uphill (and hard!) bike ride. I don’t know how to explain it, but about halfway, I experienced a sharp pounding sensation in my head and all of my muscles suddenly stopped “working.” I couldn’t move. It was very scary and I was afraid we were going to have to call 911. But after a very long rest, we were able to head back to the condo (I was very thankful, too, that the journey back was mostly coasting down the hill). We were all so confused why that happened. That next month, I started volunteering at Providence St. Vincent’s NICU because I wanted to “cuddle” the babies.
It was very scary and I was afraid we were going to have to call 911. But after a very long rest, we were able to head back to the condo (I was very thankful, too, that the journey back was mostly coasting down the hill). We were all so confused why that happened. That next month, I started volunteering at Providence St. Vincent’s NICU because I wanted to “cuddle” the babies. Before I could start cuddling, I had to do normal NICU volunteer work like carting cribs to different floors or continually filling containers with more saline flushes, bandages, etc. The next month though, I suddenly started experiencing left-sided weakness and a left drooping eye. I had to go to the ER and later be admitted for tests after tests. I had CAT scans, a lumbar puncture, numerous EMGs, blood tests, and more. I was in the hospital for 9 days and was tested for Lambert-Eaton Syndrome, more severe types of Ehlers-Danlos, Myasthenia Gravis, Multiple Sclerosis, stroke, and more. I was sent home with all of the above diseases ruled out with no answer still. My pain dr. referred me to a neurologist that he knew and trusted. My neurologist really wanted me to get 4 MRIs done all at the same time (brain, cervical, thoracic, and lumbar spine) to rule out other diseases because CAT scans aren’t always reliable…..but my SCS was not MRI-compatible.
Before I could start cuddling, I had to do normal NICU volunteer work like carting cribs to different floors or continually filling containers with more saline flushes, bandages, etc. The next month though, I suddenly started experiencing left-sided weakness and a left drooping eye. I had to go to the ER and later be admitted for tests after tests. I had CAT scans, a lumbar puncture, numerous EMGs, blood tests, and more. I was in the hospital for 9 days and was tested for Lambert-Eaton Syndrome, more severe types of Ehlers-Danlos, Myasthenia Gravis, Multiple Sclerosis, stroke, and more. I was sent home with all of the above diseases ruled out with no answer still. My pain dr. referred me to a neurologist that he knew and trusted. My neurologist really wanted me to get 4 MRIs done all at the same time (brain, cervical, thoracic, and lumbar spine) to rule out other diseases because CAT scans aren’t always reliable…..but my SCS was not MRI-compatible. My pain dr. felt deep down that the MRIs would be normal, but because he trusted my neurologist, I had another surgery to have my spinal cord stimulator explanted (removed). It was a sad day. And when we later found out that the MRIs didn’t give any answer as to what was causing my muscle weakness, drooping eye, and other new symptoms like fatigue (I started sleeping more than 14 hours per day), headaches, muscle jerking, and much more, I broke down and wept.
My pain dr. felt deep down that the MRIs would be normal, but because he trusted my neurologist, I had another surgery to have my spinal cord stimulator explanted (removed). It was a sad day. And when we later found out that the MRIs didn’t give any answer as to what was causing my muscle weakness, drooping eye, and other new symptoms like fatigue (I started sleeping more than 14 hours per day), headaches, muscle jerking, and much more, I broke down and wept.
2013: In April, my parents, sis, and I traveled all the way to Cincinnati Children’s Hospital because it’s a top Children’s Hospital and also because we still didn’t have any answers. I saw the Genetics team, and in addition to confirming my Ehlers-Danlos (EDS), they suspected that I could possibly have a Mitochondrial disorder. We started reading up about it, and as I began to have more and more concerning neurological symptoms and GI dysmotility, mito seemed like it could be THE answer (since mito “red flags” are if you have symptoms in 3 or more organs). My parents and I went back to Cincinnati Children’s at the end of 2013, and I saw many more teams like Cardiology, Pulmonology, Neuro-gastroenterology, and Genetics again. Because the genetics team wasn’t an expert in Mitochondrial Medicine, they referred me to a top mitochondrial specialist at UCSD in San Diego.
2014: I started to lose weight because my GI dysmotility was really bad….I couldn’t handle much food at all. I drank nutritional shakes and even baby food pouches, but I continued to lose, so I had to get a nasal-jejunal feeding tube placed for continuous tube feeds. In June, my parents, sis, and I headed down to see my mitochondrial specialist. We spent a week there….the evaluation was very long, and I also had to get my first muscle biopsy and a lot of genetic testing sent off at the end of that week.. It took many, many months for results to come back. In August, I had yet another surgery to get a jejunostomy feeding tube placed in my abdomen since NJ tubes are only temporary. But, a couple months later, I started to not tolerate my tube feeds because my GI dysmotility had worsened. I became malnourished, and I felt terrible. My weight dropped down to 77 pounds, so because we ran out of other options, my GI doctor had me get admitted to OHSU the day after Christmas to start TPN (IV nutrition). That’s considered a last resort because of the complications that can happen from it (blood infections due to having a central line for the TPN, liver disease, etc.), but sadly, there were no other good options.
2015: At the beginning of the year, we received some of my muscle biopsy results. We found out that I had a pretty significant mitochondrial DNA depletion which basically means that I have much less mitochondrial DNA than the normal person. My mito specialist diagnosed me with Mitochondrial DNA Depletion Syndrome. Mitochondria are the organelles that make energy for all organs to work/function, and they are in every cell of the body, except red blood cells. Because they’re pretty much everywhere in the body, that’s one of the reasons why I have soo many symptoms in numerous body systems. But, this biopsy didn’t tell us the exact gene mutation that caused this depletion. So, once again, I had to get more genetic testing done. This meant more waiting. In February, I got my first blood clot in my PICC (peripherally-inserted central catheter) line which is another complication due to TPN/central lines. I had to get the line removed, and a couple weeks later, I had surgery to have my first Groshong central line placed in my chest. The last several months of 2015, my liver function tests started getting really high, and even though my GI dr. was sure that I didn’t have another genetic disorder, I had to get a liver biopsy in November to check the copper level in my liver and rule out Wilson’s Disease. Well, to his great surprise, the biopsy confirmed that I have Wilson’s. I was so sad that I had to deal with yet another disorder. So my GI dr. referred me to a hepatologist (liver specialist).
So my GI dr. referred me to a hepatologist (liver specialist).
2016: The beginning of this year was really rough. I ended up in the ER for body pain all over and other symptoms. I was diagnosed with Hypomagnesemia and had to add yet another specialist to my long list—a nephrologist. When I saw the kidney specialist and had more tests, we found out what was causing the hypomagnesemia. I had renal magnesium wasting….in other words, my kidneys weren’t holding on to Mg which was then causing the low Mg levels. I had to get 8 GRAMS of IV magnesium for 5 hours every day, along with 16 hours of TPN every night. It was so hard being hooked up to an IV pump pretty much the whole day. After that ER visit, I still was feeling really ill. When I was finally able to see the liver specialist, I had acute hepatitis from the Wilson’s….so I was started on continual zinc therapy which is a chelating agent (it blocks the body from not absorbing any more copper). In March (a year and one month since my central line placement), I experienced sepsis for the first time, and we found out I had a blood infection (staph capitis) from my central line. I had to get the line removed and have surgery to place a new line on the other side of my chest. In August, I had surgery on my left hip to repair a hip labral tear. I also had another surgery at the same time—my second muscle biopsy to do more mitochondrial tests and also check up on the depletion. When we received results back, we found out that my depletion has worsened and also that my muscle had more abnormal histological changes. At the end of this year, I had a tunneled line infection which thankfully didn’t travel to my blood. But my dr. decided I should get a port placed to try and prevent me from having a blood infection every year (a port works the same way as a central line but you have to get poked every time to get blood drawn). My GI dr. told me that ports are known to cause fewer blood infections.
2017: At the beginning of the year, I had a DVT (deep vein thrombosis) near my central line. The doctors weren’t sure if I could get my port placed because they didn’t want the clot to travel to my heart (all central lines/ports lead to the heart). They consulted a top Hematology expert who said it would be fine to still have the surgery. I had the port surgery, and just 5 months later, I became septic again from a port blood infection due to Staph Epidermidis. What irony since ports are “supposed” to cause less infections. But I guess my doctors should have expected this since I don’t follow “protocol” in pretty much any medical thing..
But I guess my doctors should have expected this since I don’t follow “protocol” in pretty much any medical thing.. So I had to have surgery to get the port removed and another surgery to place a Hickman central line.
So I had to have surgery to get the port removed and another surgery to place a Hickman central line.
2018: In August, I had my second hip surgery to repair another hip labral tear on the right side (my other labral tear surgery in 2016 was on the left side). And 24 hours after that, I went into septic shock for the first time, the Rapid Response Team came, and I had to be rushed to the ICU. My blood pressure got dangerously low, so they had to give me Norepinephrine. My kidneys and liver took a big hit. I got ischemic hepatitis, and my liver enzymes skyrocketed to over 900 (normal is below 40). Anyways, if you want to know what else happened then, you can go back to that blog post. That was such a very scary and traumatic time.. It was a bad highlight of the year, but the wonderful highlight was going to Disneyworld in February with my whole family for the first time. It was an amazing “make a wish” type of gift from some dear family friends.
That was such a very scary and traumatic time.. It was a bad highlight of the year, but the wonderful highlight was going to Disneyworld in February with my whole family for the first time. It was an amazing “make a wish” type of gift from some dear family friends.
And now, this leads me to this past year 2019:
At the end of January, I had to go to the ER and was diagnosed with sepsis again, but they couldn’t figure out what was causing it (we later learned from an OHSU immunologist that it is common to sometimes not be able to find the cause). I was in the hospital for 11 long days, my longest hospital stay to date. This stay and the ICU stay in 2018 were both the hardest ever (even more than the 2 sepsis episodes in 2016 and 2017)….I wept profusely on my hospital bed and cried out to God. But this whole post is already getting super long, so you can find that blog post to see what happened if you want. Would you like to hear some good news, though? I haven’t had a hospital stay or ER visit since then. What a praise, and all glory goes to God!
Would you like to hear some good news, though? I haven’t had a hospital stay or ER visit since then. What a praise, and all glory goes to God!
But, since the middle of November, some of my labs started looking abnormal. And now, as I write this, my Manganese, Triglycerides, ALT and AST (liver enzymes), GGT (another liver test), and Phosphorus are all high (maybe I’m forgetting some?). I’ve been feeling off, my eyes are really droopy, the pain’s been so bad, I’ve been experiencing more GI symptoms, dizziness, itching, and something just isn’t right. I saw my GI specialist, and of course, he says I’m not the typical patient and he’s not sure what’s going on. So he ordered blood cultures (he doubts a blood infection but still wants to have that ruled out) and soo many other blood tests to check for liver diseases, autoimmune things, and a specific genetic disorder that affects the liver. Here’s all the blood I had drawn today..
I saw my GI specialist, and of course, he says I’m not the typical patient and he’s not sure what’s going on. So he ordered blood cultures (he doubts a blood infection but still wants to have that ruled out) and soo many other blood tests to check for liver diseases, autoimmune things, and a specific genetic disorder that affects the liver. Here’s all the blood I had drawn today..

He also ordered a specialized liver ultrasound called a FibroScan (transient elastography). Would appreciate prayers that it can be done within the next week. Because if the scan is normal, he will consider a liver biopsy to be done the same time I have my foot surgery (to remove that vascular malformation which grew back in the bottom of my right foot) and j-tube replacement on January 15th.
I recently received some more disappointing and sad news. When I saw my mito specialist in July, he told us about a specific mitochondrial drug trial in Phase 2 that was doing really well, and he hoped it would be FDA approved within a couple of years. Well, we found out that it didn’t pass Phase 3 and meet certain endpoints. I was so hopeful that this drug could help me, and now I realize that maybe I was putting too much hope in it. I read an encouraging quote by Paul David Tripp in his devotional New Morning Mercies. He shared about Romans 5:1-5 which talks about suffering and hope. He wrote, “Vertical hope (hope in God) will never put us to shame. This means that all other forms of hope (which he calls “horizontal hope”)
fail us in some way. Hope in created things never delivers what hope in the Creator can.” And that is so true.
I was so hopeful that this drug could help me, and now I realize that maybe I was putting too much hope in it. I read an encouraging quote by Paul David Tripp in his devotional New Morning Mercies. He shared about Romans 5:1-5 which talks about suffering and hope. He wrote, “Vertical hope (hope in God) will never put us to shame. This means that all other forms of hope (which he calls “horizontal hope”)
fail us in some way. Hope in created things never delivers what hope in the Creator can.” And that is so true.
As you can see, this past decade has been so hard. SO VERY HARD. I’ve lived with chronic pain for 10 years now, I’ve had countless ER and hospital stays throughout the years. I still can’t drive. I have doctor appointments on end. I’ve been poked and prodded and have had horrible procedures/surgeries and invasive tests (I’m having surgery #21 in a couple weeks, Lord willing). I still can’t work (other than my little job with Punkpost which is a huge blessing from God).
But you know what? I don’t want you to feel sorry for me. I don’t want your pity. But I do want you to know that I truly couldn’t haven’t survived these past 10 years without my Lord and Savior, Jesus Christ, by my side. I could be angry at Him. I could be depressed. I could feel like life has no purpose or meaning. But because of Him, I do have purpose in the pain. He is my Rock, and He has carried me through all of these past 3,650 days. And I know He will be there for me the next 10 years as well. The Lord is so good and so faithful to me, and I’m so thankful that “God’s goodness doesn’t change based on the condition of my circumstances” (unknown author).
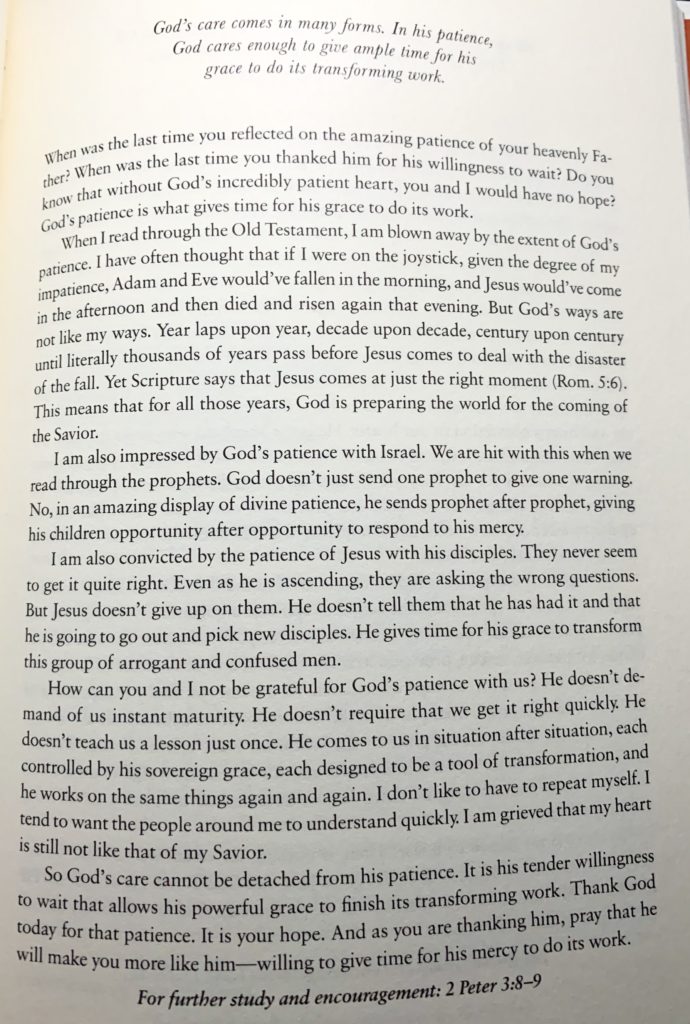
To end (which might possibly be my longest blog post to date ), I want to say one more thing that I’ve learned about the Lord this past decade. He is so patient to me and with me. Patient when I’m emotionally spent. Patient when I’m not patient with others. Patient when I’m upset. Patient when I’m sometimes sad or discouraged. Patient when I’m impatient waiting for tests or wheelchair supplies or surgeries or pain meds to get pre-authorized by my insurance. And when I had a day where I was really struggling with patience, I read this excerpt that very night from the same devotional New Morning Mercies. It almost brought tears to my eyes. And I want to share it with you. Please read it. The last paragraph in it meant so much to me, especially. I hope it encourages you immensely.
), I want to say one more thing that I’ve learned about the Lord this past decade. He is so patient to me and with me. Patient when I’m emotionally spent. Patient when I’m not patient with others. Patient when I’m upset. Patient when I’m sometimes sad or discouraged. Patient when I’m impatient waiting for tests or wheelchair supplies or surgeries or pain meds to get pre-authorized by my insurance. And when I had a day where I was really struggling with patience, I read this excerpt that very night from the same devotional New Morning Mercies. It almost brought tears to my eyes. And I want to share it with you. Please read it. The last paragraph in it meant so much to me, especially. I hope it encourages you immensely.
May we all continue to be strong in the Lord and in His mighty power this new year, friends. I love you and am so thankful for your faithful prayers and for just being on this long journey with me.




