Sepsis….a second time. And news on baby Charlie Gard.
Hi friends,
Wow!! So much has happened, but I will just go right in and try to tell you everything..
The last week of June, I started feeling very
off with episodes of nausea and severe head pain (not my “normal”) all over….it even hurt to move my eyes. So on Tuesday the 27th, I decided to check my temperature. It was 100.9 degrees…I thought that was weird and wondered if it was registering correctly. The next day, my nurse came over for my weekly blood draw and port needle/dressing site change. She checked my vitals like she always does. If I remember correctly, my temp showed that it was 101.8 with her temporal thermometer. So to make sure, she checked my temp again but this time with her tympanic (ear) thermometer. It registered as 102.1. She was not expecting that. She even checked my temp again with my own thermometer, and it was 102.4. I told her everything and how I was feeling terrible, so she called the nurse on-call at my GI doctor’s office. Because the clinic was almost closing by that time, my GI dr. recommended that I go to the ER in case I had an infection from my port.
So on Tuesday the 27th, I decided to check my temperature. It was 100.9 degrees…I thought that was weird and wondered if it was registering correctly. The next day, my nurse came over for my weekly blood draw and port needle/dressing site change. She checked my vitals like she always does. If I remember correctly, my temp showed that it was 101.8 with her temporal thermometer. So to make sure, she checked my temp again but this time with her tympanic (ear) thermometer. It registered as 102.1. She was not expecting that. She even checked my temp again with my own thermometer, and it was 102.4. I told her everything and how I was feeling terrible, so she called the nurse on-call at my GI doctor’s office. Because the clinic was almost closing by that time, my GI dr. recommended that I go to the ER in case I had an infection from my port.
I really didn’t want to go as I had 2 ER visits (see previous post) already that month alone! But because I was feeling so bad, we agreed to head back to the ER. I beat my record for most ER visits in a month! haha Just to double-check once again, I checked my temp right before my mom and I left the house, and it was 102.7.
Just to double-check once again, I checked my temp right before my mom and I left the house, and it was 102.7.
Thankfully, there was hardly any wait time when we arrived. I had several tubes of blood drawn, and the doctors also ordered a chest x-ray and urinalysis to rule out a bladder infection. The x-ray and urine tests were completely normal, so the doctor prepared me with the news that I would most likely be admitted as blood cultures take up to 48 hours (or longer) to grow.
Sadly, the hospital had no rooms available, so my first night there was spent in the ER. I was hooked up to monitors because I had a very high heart rate. I also had lots of IV fluids running. I was very sleepy and felt so sick from whatever was going on. The hospital medicine dr. who came to the ER to consult said I was septic….
I couldn’t believe that my port got infected after only 5 months!
The hospital medicine dr. who came to the ER to consult said I was septic….
I couldn’t believe that my port got infected after only 5 months!
It got placed in January….and we now know that a port is not the best kind of vein access for me because I have to get accessed every single day for my IV infusions….this meant that the port needle had to stay in my chest all the time which is a higher risk for infection, even though the needle did get changed once a week. You may think, “Doesn’t a regular central line stay in all the time, too?” Yes, it does, but it’s not pulled out and a new one isn’t inserted every week like a port needle…each time a port needle is inserted, there’s a higher chance for bacteria to get inside…hope that makes sense. :/ Usually, patients with ports aren’t accessed every day…they may use it a few days in a week, but then the needle gets removed for a little while afterwards and is not used at all.
But back to the story.. The doctors now were just waiting for the cultures to grow to see what kind of bacteria this was. And before even 48 hours went by, my blood cultures from my port started growing Staphylococcus Epidermidis. Even my blood directly grew this bacteria which was not good at all.
The doctors now were just waiting for the cultures to grow to see what kind of bacteria this was. And before even 48 hours went by, my blood cultures from my port started growing Staphylococcus Epidermidis. Even my blood directly grew this bacteria which was not good at all.
At around 6 AM, I was moved to a room on 14A, and I was so grateful that it was a private one! It even had a beautiful view (see picture above)!
The infectious disease team started caring for me in addition to the hospitalists….they put me on 2 very aggressive IV antibiotics. Early each morning around 3:30-5:30 AM, I had to get poked for blood work. IV therapy also had to place IVs in both of my arms because the IV antibiotics (along with my regular IV nutrition and magnesium) were so hard on my veins. It was extremely painful to infuse such strong medications in my small veins.
On Monday (7/3), the infectious disease specialist called my GI dr. to see if there was any way I could get off TPN and just do tube feeds, but my GI dr. explained how I couldn’t stop it at all because I need the nutrition, IV fluids, and magnesium.
Even while I was inpatient, the doctors ordered something called a “calorie count” to see how many calories I eat orally in a day. They figured out that I eat around 500 calories on average per day, and I would need to eat much more than twice that to not need TPN.
At first, Infectious Disease wanted to try and save my port (i.e., not remove it) because needing to remove and replace ports/lines means less and less vein access down the road due to scar tissue, but after consulting with my GI dr. and the hospitalists, they all agreed that it was best to remove it and place a new central line.
I had surgery that afternoon to remove my port. It turned out to be the right decision after all—they cultured the port catheter tip, and it still came back positive for S. Epidermidis, even though I continued to be on the strong IV antibiotics. The port surgery was rough as I had to be awake for it. My surgeon took a picture of my chest incision, and I would share it here, but it’s graphic. haha
My surgeon took a picture of my chest incision, and I would share it here, but it’s graphic. haha
Long story short, I was in the hospital for a total of 9 days. I had surgery #16 on 7/5 to place a new Hickman central line. I love my new line! And I pray it lasts much longer than 5 months.
And I pray it lasts much longer than 5 months.
This is the second time I’ve had sepsis due to a central line-associated bloodstream infection (Staphylococcus Capitis grew in my blood last year), and I wonder if it will happen once a year from now on.. My doctors said it’s not a matter of “if” but “when” it will get infected again. But I’m comforted as I know the Lord is with me every single day….my life is in His hands. And I trust Him with my future.
My doctors said it’s not a matter of “if” but “when” it will get infected again. But I’m comforted as I know the Lord is with me every single day….my life is in His hands. And I trust Him with my future.
I got discharged on 7/6, and I’m still doing a long routine of IV antibiotics 3x a day. It’s so rough, and I’ve been experiencing bad vertigo as a side effect of the antibiotic. I have to wake up at midnight each day, start the antibiotic infusion, then wake up again at 1 AM to stop the infusion. Then I have to wake up at 8 AM and do the whole routine again. At 4 PM, I once again start the antibiotics, stop them one hour later, etc. I can’t wait to be finished!!
I have to wake up at midnight each day, start the antibiotic infusion, then wake up again at 1 AM to stop the infusion. Then I have to wake up at 8 AM and do the whole routine again. At 4 PM, I once again start the antibiotics, stop them one hour later, etc. I can’t wait to be finished!!
I’m so thankful I didn’t have doctor appointments this week as our upstairs bathrooms are getting remodeled (it’s so very loud, and I don’t get my normal rest) on top of all this. Next week, I do see my physical medicine dr. and my GI specialist..
Here are a few photos of my hospital stay. I already shared some on FB, but I’ll post them here as well for those who haven’t seen them. Thank you for reading this super long post!
I already shared some on FB, but I’ll post them here as well for those who haven’t seen them. Thank you for reading this super long post! And thank you so much for praying for me.
And thank you so much for praying for me.
P.S. I’m so thankful that the courts
are now allowing Dr. Hirano
(an expert in mitochondrial disease who practices in New York….I met him last year at the UMDF symposium, and he looked at one of my test results.. ) to see and evaluate baby Charlie Gard
in the U.K. This story keeps on hitting so close to home because I have a mitochondrial DNA depletion syndrome like baby Charlie (I have a different type, tho). Feel free to read these links that I highlighted to learn more about this precious baby. Continuing to pray for little 11-month old Charlie and his parents!
) to see and evaluate baby Charlie Gard
in the U.K. This story keeps on hitting so close to home because I have a mitochondrial DNA depletion syndrome like baby Charlie (I have a different type, tho). Feel free to read these links that I highlighted to learn more about this precious baby. Continuing to pray for little 11-month old Charlie and his parents! #iamcharliegard #charliesfight
#iamcharliegard #charliesfight

taking a short walk for the first time this hospital admission
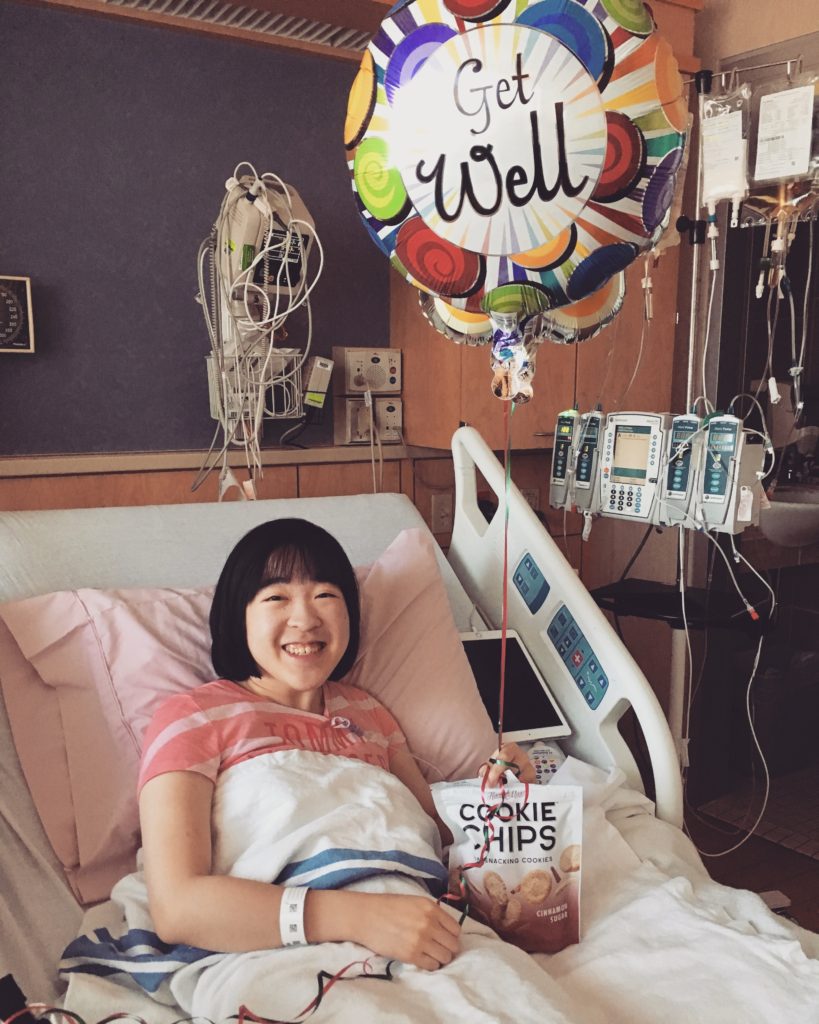
my mom and dad surprised me with balloons and a treat!

a therapy dog came to visit me, and it was so much fun!

my IV and tube feeding pumps.

feeling sore after having my new central line placed.

this is what my IV antibiotic looks like! lol




