Mitochondrial genetics appointment.
Hello friends,
My family and I got back from CA on Sunday. It was a super quick trip, but we were able to spend a lot of time together which was so special.
Our first two evenings there, I suddenly had terrible nausea and severe muscle weakness to the point that I couldn’t lift my arms or even get up to brush my teeth. All I could do was lay on the hotel bed. It was even so hard to hold my phone up. I couldn’t help crying because it was scary. This didn’t happen at all when my parents and I traveled to San Diego in January. I hate that I’m getting worse and feeling the disease progression. :'( If I were home, I would have had to go to the ER. At one point, I thought I’d need to go to the hospital in LA. We don’t exactly know what caused these episodes—maybe a combination of very low blood sugar (despite being hooked up to my regular tube feeds and IV fluids), exhaustion from not getting enough rest, etc. So for the rest of the trip, my family mainly pushed me in my chair (instead of me “wheeling” myself) so that I could save energy. When we went to Universal Studios on Friday and Saturday, I didn’t wake up till the afternoon so that I would have enough strength.
I couldn’t help crying because it was scary. This didn’t happen at all when my parents and I traveled to San Diego in January. I hate that I’m getting worse and feeling the disease progression. :'( If I were home, I would have had to go to the ER. At one point, I thought I’d need to go to the hospital in LA. We don’t exactly know what caused these episodes—maybe a combination of very low blood sugar (despite being hooked up to my regular tube feeds and IV fluids), exhaustion from not getting enough rest, etc. So for the rest of the trip, my family mainly pushed me in my chair (instead of me “wheeling” myself) so that I could save energy. When we went to Universal Studios on Friday and Saturday, I didn’t wake up till the afternoon so that I would have enough strength.
Regarding the appointment, my mitochondrial geneticist spent 3 1/2 hours with me!! He is amazing and so knowledgeable. He hasn’t seen a new patient in more than a year because he mainly travels across the US and teaches doctors about gene sequencing and more, but he wanted to see me because I stood out to him! So grateful to be under his care!
So grateful to be under his care!
In a nutshell, he explained that I have a multi-factorial (polygenic) mitochondrial disease which means it’s not just one gene mutation causing the disease—it’s a combination of gene variants that are contributing to my symptoms. He believes the CHAT variant I have is modifying the TRAP1 (TNF receptor-associated protein 1) gene. In his words, TRAP1 is a mitochondrial chaperone that is believed to protect mitochondria from the effects of reactive oxygen species-related damage. Having CHAT and TRAP1 together is much worse than if I just had one or the other. He said patients with both are in bad shape. I have intestinal failure and many other things going on. He agrees that my mitochondrial disease is progressive. In his practice, 90% of his patients improve or stabilize with his treatment and 10% don’t…
He’s putting me on high-dose co-factors (antioxidants) and supplements. He wants my blood CoQ10 level and blood “free and total” carnitine level checked. Normal blood CoQ10 is under 4, but he wants my level to be way above 4 because he has found that a higher level is much more effective to help. Once I email him the blood results, he will tell exactly how much of each antioxidant I need to take.
He stated that I shouldn’t go more than 2 hours without eating because fasting makes everything worse.
He also wants a migraine genetic panel done through this certain lab that is a division of Courtagen Life Sciences (he’s the medical director of Courtagen, and I had gene sequencing through them). There are many genes (including pain genes) on this panel that I haven’t had sequenced before. And the results will tell him exactly what migraine treatment is good for each variant that is found.
He wrote up a very long report for me and my doctors which is so helpful! He wanted to see me back in 6 months, but we’ll see him in a year instead because it gets expensive traveling and because I still see my mito dr. in San Diego.
Here are few pictures from the trip. Some of these I already posted on FB, but I know some of you aren’t on, so I wanted to share them here!
Some of these I already posted on FB, but I know some of you aren’t on, so I wanted to share them here!

me and my siblings
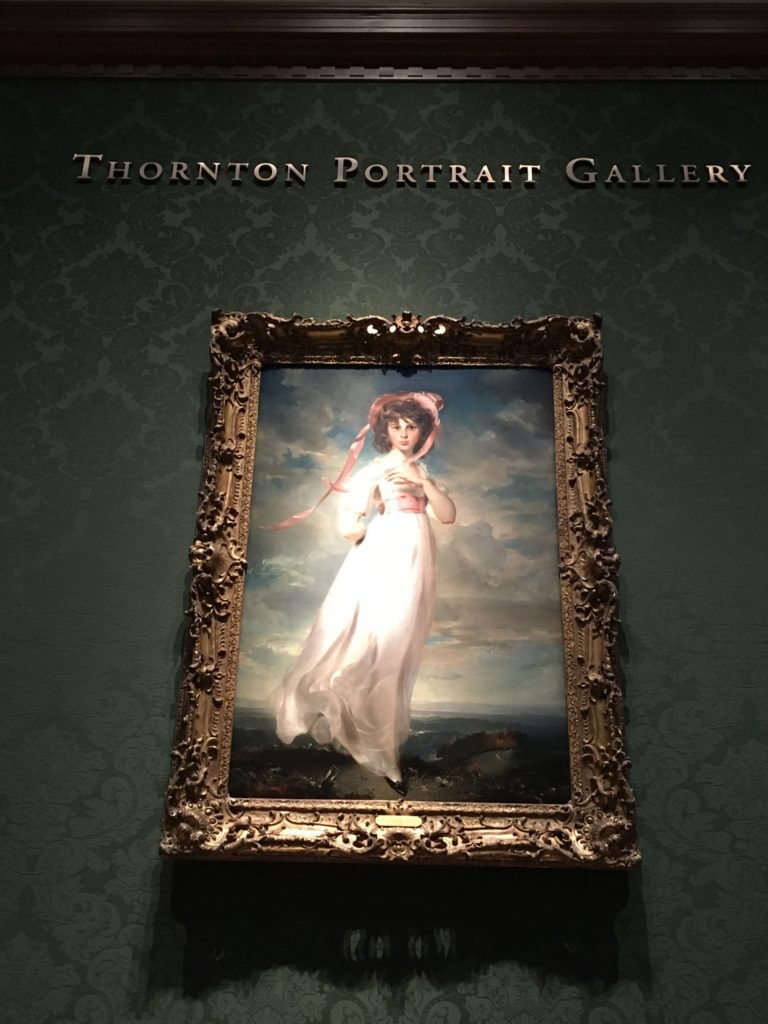
My GI dr. told me to find these two famous paintings in the Huntington Library known as Pinkie and the Blue Boy. They face each other from across the room!

The Blue Boy


The Huntington Library and Botanical Gardens in Pasadena was a highlight of the trip!!
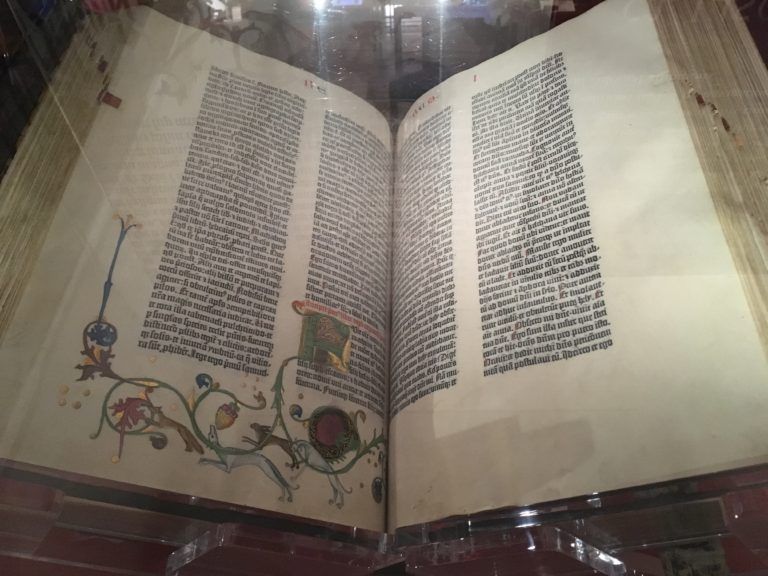
the Gutenberg Bible!!

My family and I had a blast at Universal! It was so much fun, and we didn’t have to wait in line much at all because they let us use the front-of-line access since I’m in a chair! That was a huge blessing!
That was a huge blessing!
_______________
Today, I had a follow-up with my PCP. She is going to order the migraine panel that my mito geneticist wants done. She is also going to talk to my nephrologist and GI specialist to see about adding D5 (dextrose) to my daily IV Magnesium bags. Hopefully it helps prevent those weakness episodes (as I had another episode a couple days after we got home) since the body can get energy fast from dextrose infused directly into the bloodstream. Waiting to hear if my neurologist can order the blood tests. In 2 weeks, I see my GI specialist again. And tomorrow, I resume physical therapy.. Thank you for all your caring comments and continued prayers, especially after my previous post! I love you all!




